Each household deserves reproductive selections, together with an opportunity at parenthood. For households fighting infertility, in vitro fertilization (IVF) serves as a promising path. However this hope usually comes with the prohibitively costly price ticket of $20,000 per cycle, and a nationwide common of two.5 cycles to have a wholesome child.
Though current alerts seem blended, the Trump Administration had initially thought of classifying IVF as an “important well being profit” beneath the Inexpensive Care Act (ACA), trying to satisfy a marketing campaign promise that it might lead a transformative shift in reproductive healthcare and handle troubling demographic developments. It parallels efforts in Congress by Democrats, who launched H.R. 3480, the Well being Protection for Inclusive and Valued Households Act of 2025, equally looking for to broaden fertility remedy entry to extra households. What these plans fail to deal with is what occurs while you stoke demand with out growing provide, inevitably resulting in a rollout that will additional improve the price of IVF with out including important capability.
Let’s look simply at Medicaid, which covers about 18 million girls aged 20-45, accounting for 40% of all U.S. births. If IVF entry have been provided to this inhabitants by way of insurance coverage protection extension, based mostly on current averages, we would count on 2% of that cohort to pursue remedy, leading to roughly 360,000 further cycles yearly. For context, in 2023, U.S. fertility clinics reported performing over 430,000 IVF cycles.
And naturally, if insurers adopted go well with, the issue would compound. We have to put downward worth stress whereas maintaining centered on high quality outcomes.
Traditionally, that’s been the other end result of including protection by way of the American medical insurance trade. Why ought to we count on any completely different if its scope have been expanded to cowl IVF? Let’s give you a greater mannequin, one thing akin to LASIK, the place costs have come down 30% since 2008, with out sacrificing high quality.
The infrastructure hole
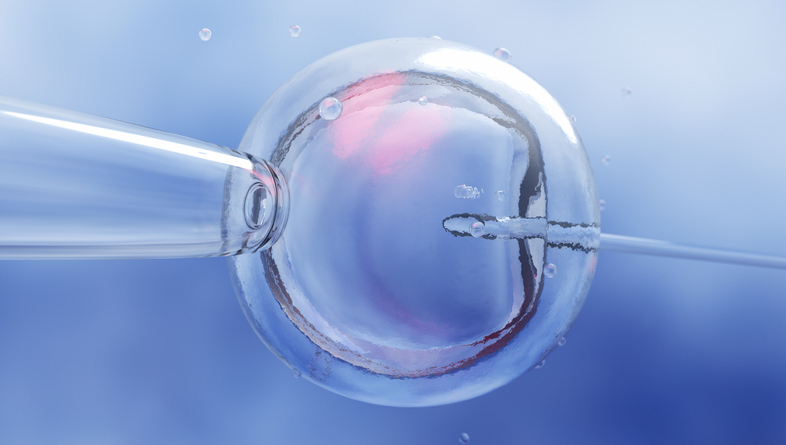
Probably the most important problem going through any large-scale enlargement of IVF protection is the acute scarcity of crucial infrastructure and specialised personnel. Not like routine outpatient care, IVF is a extremely intricate and manually intensive process that includes a number of phases, from ovarian stimulation and egg retrieval to fertilization, embryo tradition, and switch. Every of those steps should be executed with extraordinary precision in tightly managed lab environments. IVF remedy is uniquely depending on a slim cadre of extremely expert professionals, most notably embryologists. These specialists are accountable for dealing with eggs, sperm, and embryos at a mobile stage, usually making split-second selections that may decide the end result of a cycle. In accordance with trade information, there are solely about 1,500 board-certified reproductive endocrinologists and roughly 5,000 embryologists actively working within the nation. In the meantime, the variety of accredited coaching packages for embryologists in america is restricted, and certification can take a number of years.
These figures have remained comparatively stagnant over the previous decade regardless of rising demand. This bottleneck has led to capability constraints, most seen outdoors of huge city facilities. Whereas metropolitan areas like New York, Los Angeles, and Chicago might have a number of full-service fertility clinics, rural and underserved areas usually lack sufficient certified people and correctly outfitted services. Some states have a single IVF clinic.
This geographical imbalance leads to lengthy wait occasions and journey burdens, significantly for these in lower-income or medically underserved communities. And given the extremely handbook nature of many delicate steps, the method has change into artisanal, with a worrisome inconsistency in high quality and outcomes between clinics, between skilled and inexperienced embryologists, and between well-rested and overworked employees.
Addressing entry
All this raises critical fairness considerations for all the steered “fixes”: increasing insurance coverage protection for IVF with out first addressing the underlying infrastructure shortfall may very well widen the hole between those that can entry fertility care and people who are merely entitled to it on paper.
If insurance coverage protection mandates result in a sudden improve in demand for IVF companies, many clinics – already stretched fairly skinny – might battle to accommodate the inflow of latest sufferers. This can lead to longer wait occasions for appointments, diagnostic testing and remedy cycles, doubtlessly delaying sufferers’ potential to begin or full fertility remedies. For people and {couples} going through infertility, such delays are particularly distressing due to the decline in fertility with age.
As well as, even when protection is remitted, insurance coverage will do nothing to decrease systemic prices – the truth is, the historical past of U.S. medical insurance suggests the other.
To really broaden entry, we have to concentrate on assuaging the bottlenecks in a manner that throwing cash on the drawback can not repair. Meaning sturdy, parallel investments in workforce improvement, recruitment incentives, and clinic infrastructure. Nonetheless, within the best-case eventualities, these are longer-term tasks that gained’t sustain with the anticipated development in demand for IVF on account of altering demographics – right here and globally.
The lacking piece is modernizing the expertise utilized in IVF, particularly automation. If correctly carried out, automation alone may assist to standardize high quality in just a few methods. It could shrink the burden on employees by decreasing the variety of handbook steps, and permit these with much less expertise to carry out procedures on par with those that have spent a profession doing them. It could speed up sure procedures and eradicate course of failures.
Automated potential
A superb instance is the method of fertilization itself, requiring a fragile handbook protocol often known as ICSI that dangers ruining a possible embryo when sperm is pressured into an egg. It may possibly take months to study and years to change into proficient. Newer expertise known as piezo-ICSI makes the injection course of gentler, leading to higher high quality eggs and blastocytes. Automated piezo-ICSI robots have lately entered the market, which simplify the method in order that less-experienced embryologists can carry out the complicated process in addition to specialists.
Bettering the general high quality of processes would result in higher outcomes, bringing down that 2.5-IVF cycle common we see at present. Having extra wholesome infants with fewer cycles will shortly unlock extra systemic capability.
Going a step additional: automation has probably the most influence when it goes past merely optimizing steps with robots. Artistic design can change paradigms. Have a look at the extremely handbook and delicate step of vitrification, the place eggs are fastidiously frozen for later use. As extra younger professionals resolve to delay beginning a household till later in life, egg freezing is an more and more crucial element of reproductive planning. However like different complicated steps, it should be carried out in a managed embryology lab setting, at a specialised IVF clinic. For anybody questioning why we don’t have extra clinics in additional locations: they price about $4 million to open and $1 million to function yearly.
Newer platforms are reaching the market that may automate vitrification in a tabletop system, with minimal, non-expert coaching required. As these change into widespread, they promise to broaden entry a lot additional. We see a world coming quickly the place these gadgets are commonplace in OB/GYN places of work, which themselves are distributed rather more broadly and nearer to the place sufferers are positioned.
Whether or not we broaden insurance coverage protection or not, there are many issues the federal government can do to convey down the out-of-pocket prices of IVF. For instance, selling biosimilars – already obtainable in Europe – for the cocktail of hormones wanted to stimulate ovulation would scale back per-cycle prices by as a lot as a 3rd. However price isn’t the core limitation to entry; it’s a symptom. If we fail to deal with provide constraints, government-mandated insurance coverage protection will change into simply one other subsidy for insurers, with out making a dent within the rising demand for IVF.
Photograph: luismmolina, Getty Photographs
Hans Gangeskar is CEO of Overture Life, a fertility expertise firm automating embryology lab processes to scale back prices and lift IVF success charges.
This publish seems by way of the MedCity Influencers program. Anybody can publish their perspective on enterprise and innovation in healthcare on MedCity Information by way of MedCity Influencers. Click here to find out how.